Depression Research
Depression (known as major depression or major depressive disorder) is a type of mood disorder characterized by a prolonged melancholic state. Various hypotheses regarding the molecular mechanisms of the onset of depression have been proposed, including the monoamine hypothesis and the brain-derived neurotrophic factor (BDNF) hypothesis, all of which are disputed.
Fujifilm Wako have a lineup of products that contribute to the elucidation of the onset mechanism of depression and development of therapeutic agents, including an ELISA kit that can specifically measure mature BDNF.
More Information
What Is Depression?
Depression, also known as major depression or major depressive disorder, is a type of mood disorder characterized by a prolonged melancholic state. Another mood disorder is bipolar disorder (manic depression), characterized by repeated bouts of manic and depressive states, which, however, is distinguished from major depression. The main symptoms of depression are depressed mood (melancholy, heavy mood) and lack of enjoyment of activities / lack of interest in anything (anhedonia and lack of motivation), with concomitant symptoms such as easy to tire (fatigability), inability to sleep / excessive sleepiness (sleep disorder), and remorse (a sense of guilt). While depression is a disease experienced by approximately 10% of the general population at least once in their lifetime1), some patients suffer long-term job absences or suicide attempts; various studies have been conducted to establish early diagnosis and treatment.
Depression is a disease that develops in conjunction with a wide variety of factors, such as stress. Various hypotheses regarding the molecular mechanisms of the onset of depression have been proposed, including the monoamine hypothesis, the hypothalamic-pituitary-adrenal (HPA) axis disorder hypothesis, the neuroinflammation hypothesis, and the brain-derived neurotrophic factor (BDNF) hypothesis, all of which are disputed.
Molecular Mechanisms of Depression
We describe hypotheses that have been proposed regarding the molecular mechanisms of the onset of depression.
Monoamine hypothesis
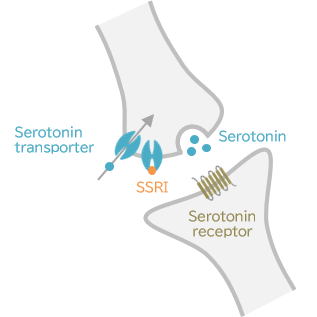
Action mechanisms of SSRIs
An SSRI inhibits the reuptake of serotonin by its transporters and increases intersynaptic serotonin concentrations.
The monoamine hypothesis assumes that depression is caused by reductions in the brain concentrations of monoamines (serotonin, noradrenaline, dopamine). As the anti-tuberculous drug iproniazid and the antihistamine imipramine were found to have antidepressant effects, and iproniazid inhibits monoamine oxidase (MAO), while imipramine inhibits serotonin and noradrenaline transporters, the monoamine hypothesis was proposed.
The monoamine hypothesis plays a central role in the molecular mechanism for depression, and many currently available antidepressants have been developed based on this hypothesis. With relatively few adverse drug reactions, selective serotonin reuptake inhibitor (SSRIs) and selective serotonin-noradrenalin reuptake inhibitors (SNRIs) are the first choice antidepressant drugs in Japan.
However, some findings cannot be explained by the simple monoamine hypothesis, including the fact that obtaining a therapeutic effect from antidepressants takes several weeks, despite monoamine levels rising dramatically after antidepressant administration2); it is anticipated that the mechanism will be clarified in more detail.
HPA axis disorder hypothesis
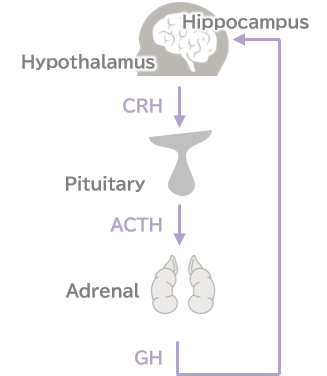
Hypothalamic-pituitary-adrenal (HPA) axis
This hypothesis assumes that stress reactions are mediated by the HPA axis, and that exposure to severe stress causes excessive signaling in the HPA axis, which in turn has adverse intracerebral effects on the hippocampus, resulting in the onset of depression.
When humans are stressed, corticotropin-releasing hormone (CRH/CRF) is released from the hypothalamus, and CRH promotes the secretion of adrenocortical stimulating hormone (ACTH) from the hypothalamus. Glucocorticoid (GC) is secreted from the adrenal and acts on the hippocampus. A pathway for suppression of CRH release comes from the hippocampus, forming a negative feedback loop along with the HPA-axis. However, prolonged exposure to severe stress damages the neurons of the hippocampus. Administration of dexamethasone, an artificial form of cortisol (a glucocorticoid), usually suppresses cortisol secretion, and patients with depression are known not to exhibit suppression with a secretion suppression test 1). This suggests that the negative feedback loop for cortisol suppression does not function normally in depression.
It remains unknown whether suppression of HPA-axis signaling ameliorates symptoms of depression, which suppression is considered to be a potential target for antidepressants in the future.
Neuroinflammation hypothesis
In recent years, it has been increasingly known that immune responses (inflammation) in the brain are involved in depression. This fact became noteworthy with reports of high incidences of depression in patients with immune disease undergoing cytokine treatment3) and of elevated inflammatory marker levels in patients with depression4). The neuroinflammation hypothesis assumes that stress-induced inflammation induces cytokines such as IL-6 and TNF-α and causes reduced neurogenesis and a disordered HPA-axis to manifest as or aggravate depression. In addition, these cytokines are considered to have the potential to reduce serotonin, synthesized from tryptophan because they activate the pathway for the synthesis of kynurenine from tryptophan5).
BDNF hypothesis
BDNF, a member of the neurotrophic family of nerve growth factors, is known to mediate neuroprotection, neurogenesis, and synaptic plasticity in the brain.
As stress, a cause of depression, lowers BDNF levels in the hippocampus6), and stress-induced BDNF reductions are lessened in rats receiving an antidepressant for a long duration7), the involvement of BDNF in depression was suggested. In addition, an antidepressant-mediated increase in expression of BDNF was found to be delayed by about 3 weeks, rather than occurring just after administration7), so this is considered to explain the delayed therapeutic effect of antidepressants. These reports have led to the BDNF hypothesis being proposed, in which stress reduces BDNF in the brain and causes neuronal atrophy and reduced synaptic plasticity, producing the condition of depression. In addition, patients with depression reportedly have serum BDNF concentrations that are significantly lower than those in healthy subjects8); it has been reported that there is a correlation between depression severity and serum BDNF concentration; and antidepressants increase serum BDNF concentrations 9). BDNF is also expected to serve as a marker of depressive disorder.
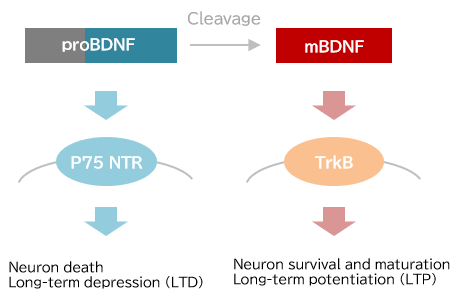
proBDNF とmBDNF
BDNF, like other neurotrophic factors, undergoes cleavage of a precursor (proBDNF) into mature BDNF (mBDNF). proBDNF and mBDNF bind to the receptors p75NTR and TrkB, respectively. proBDNF and mBDNF act reciprocally; proBDNF promotes nerve cell death and long-term depression (LTD) of synaptic transmission, whereas mBDNF promotes nerve cell survival, maintenance and maturation, as well as long-term potentiation (LTP) of synaptic transmission10).
Although no conclusion has been reached on whether proBDNF or mBDNF is effective as a marker of depressive disorder, Yoshida et al. reported that in patients with depression, serum mBDNF decreased, but proBDNF did not11). In order to understand BDNF as a treatment target or disease marker for depression, it seems necessary to differentially measure proBDNF and mBDNF.
Oxytocin and depression
Oxytocin, a nine-amino acid neuropeptide, is produced in the hypothalamus and released mainly from the posterior pituitary with labor and lactation, to promote uterine contractions and milk secretion. Since oxytocin also mediates the formation of maternal behavior and has “anti-stress” activity, it is generally called a “happiness hormone” and “love hormone.”
With regard to the association between depression and oxytocin, it is known that the duration of mouse immobility in a forced swimming test (a model of the depressive state) was shortened after administration of oxytocin, and that its effect was as substantial as that of the antidepressant imipramine12). In response to such animal study results, attempts have been made to utilize oxytocin to treat depression.
To utilize oxytocin as a depression biomarker, a study compared oxytocin levels between patients with depression and healthy individuals; however, results differed between the two sexes, and no consistent results were obtained compared with healthy persons, so further research will be required13).
References
- “Neuroscience Illustrated 3rd ed.” ed by Manabe, T., Mori, H., Watanabe M., Okano, H., Miyakawa T., Yodosha, Japan, (2013). (Japanese)
- Jeon, S. W., and Kim, Y. K.: Int. J. Mol. Sci., 17(3),381(2016).
Molecular Neurobiology and Promising New Treatment in Depression - Trojan, E., Chwastek, J., and Basta-Kaim, A.: Curr. Neuropharmacol., 14(7),705(2016).
A Potential Contribution of Chemokine Network Dysfunction to the Depressive Disorders - Uddin, M., et al.: Psychol. Med., 41(5),997(2011).
Epigenetic and inflammatory marker profiles associated with depression in a community-based epidemiologic sample - Myint, A. M., and Kim, Y. K.: Med. Hypotheses, 61(5-6),519(2003).
Cytokine-serotonin interaction through IDO: a neurodegeneration hypothesis of depression - Smith, M. A., et al.: J. Neurosci., 15(3),1768(1995).
Stress and glucocorticoids affect the expression of brain-derived neurotrophic factor and neurotrophin-3 mRNAs in the hippocampus - Nibuya, M., Morinobu, S., and Duman, R. S.: J. Neurosci., 15(11),7539(1995).
Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments - Karege, F., et al.: Psychiatry Res., 109(2),143(2002).
Decreased serum brain-derived neurotrophic factor levels in major depressed patients - Shimizu, E., et al.: Biol. Psychiatry, 54(1),70(2003).
Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants - Castrén, E., and Kojima, M.: Neurobiol. Dis., 97, 119(2017).
Brain-derived neurotrophic factor in mood disorders and antidepressant treatments - Yoshida, T., et al.: PLOS ONE, 7(8),e42676(2012).
Decreased serum levels of mature brain-derived neurotrophic factor (BDNF), but not its precursor proBDNF, in patients with major depressive disorder. - Arletti, R., and Bertolini, A.: Life Sci., 41(14),1725(1987).
Oxytocin acts as an antidepressant in two animal models of depression - Massey, S. H., Backes, K. A., and Schuette, S. A.: Depress. Anxiety, 33(4),316(2016)
PLASMA OXYTOCIN CONCENTRATION AND DEPRESSIVE SYMPTOMS: A REVIEW OF CURRENT EVIDENCE AND DIRECTIONS FOR FUTURE RESEARCH
For research use or further manufacturing use only. Not for use in diagnostic procedures.
Product content may differ from the actual image due to minor specification changes etc.
If the revision of product standards and packaging standards has been made, there is a case where the actual product specifications and images are different.
The prices are list prices in Japan.Please contact your local distributor for your retail price in your region.



